Abstract
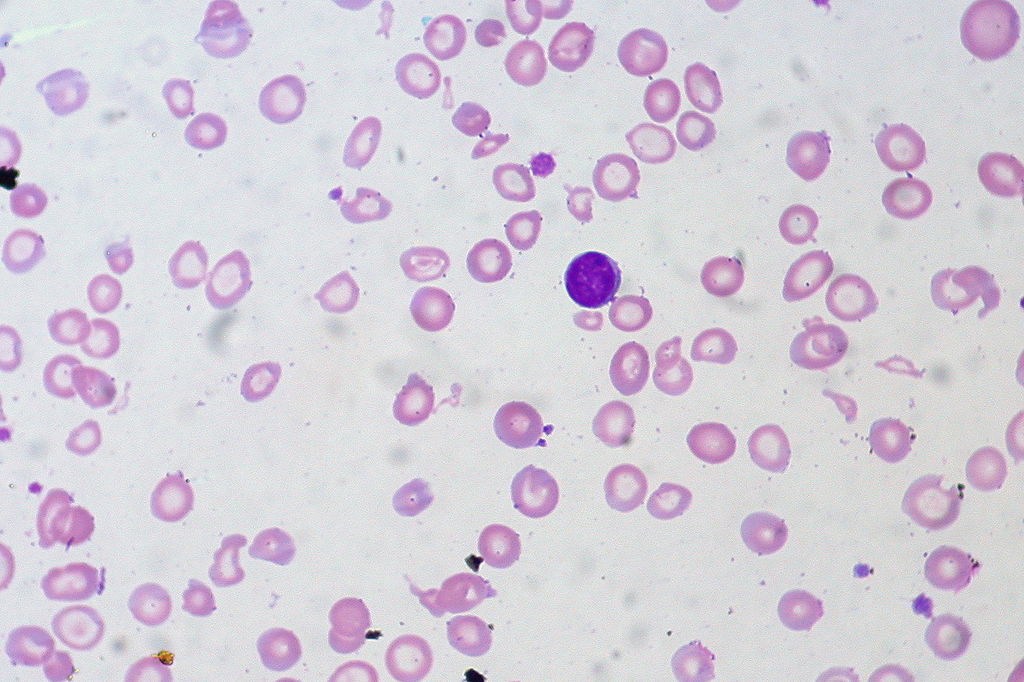
Worldwide, over 40% of children have iron deficiency anaemia, frequently associated with infections. Certain cytokines are involved in both immune activation/response to infection and iron transport/metabolism. We therefore assessed the relations among iron deficiency, cytokine production and lymphocyte activation markers in 142 hospitalized Malawian children. We examined peripheral blood lymphocyte antigens/cytokine production using four- colour flow cytometry and serum transferrin receptor (TfR) levels, an inverse measure of iron status unaffected by acute illness or infection, with an enzyme-linked immunosorbent assay. Wilcoxon rank sum tests and logistic regression analyses (LRA) were performed. Iron deficiency (TfR > or = 10 microg/ml) versus TfR < 10 microg/ml, was associated with higher percentages of lymphocytes producing: (a) induced or spontaneous IL-6 (medians: induced, 15.9% for iron-deficient children versus 8.8% for iron-replete children, P = 0.002; spontaneous, 24.4% versus 13.0%, P < 0.001) and (b) induced IFN-gamma (medians:18.4% versus 12.4%, P = 0.006). The percentages of CD8(+) T cells spontaneously producing IL-6 and of all lymphocytes producing induced TNF-alpha and IFN-gamma in the same cell had the strongest relationships to iron deficiency (b = + 0.0211, P = 0.005 and b = + 0.1158, P = 0.012, respectively, LRA) and were also positively related to the co-expression of the T cell activation markers HLA DR and CD38. Severe iron deficiency (TfR > or = 30 microg/ml) was associated with the percentage of lymphocytes producing induced IL-4 (medians: 0.5% versus 1.6%, P < 0.010). The cytokine patterns associated with iron deficiency in our study would preserve iron stores but also preferentially retain the activation capabilities of T cells, albeit not necessarily other immune cells, until a critical level of iron depletion is reached.
Jason J, Archibald LK, Nwanyanwu OC, Bell M, Jensen RJ, Gunter E, Buchanan I, Larned J, Kazembe PN, Dobbie H, Jarvis WR
Clin. Exp. Immunol. 2001 Dec;126(3):466-73
PMID: 11737064
Jason_et_al-2001-Clinical__Experimental_Immunology-iron Jason_et_al-2001-Clinical__Experimental_Immunology-iron